Encephalitozoonosis in Rabbits: Causes, Symptoms, and Treatment
Understanding E. cuniculi infection in rabbits: diagnosis, treatment options, and prevention strategies.
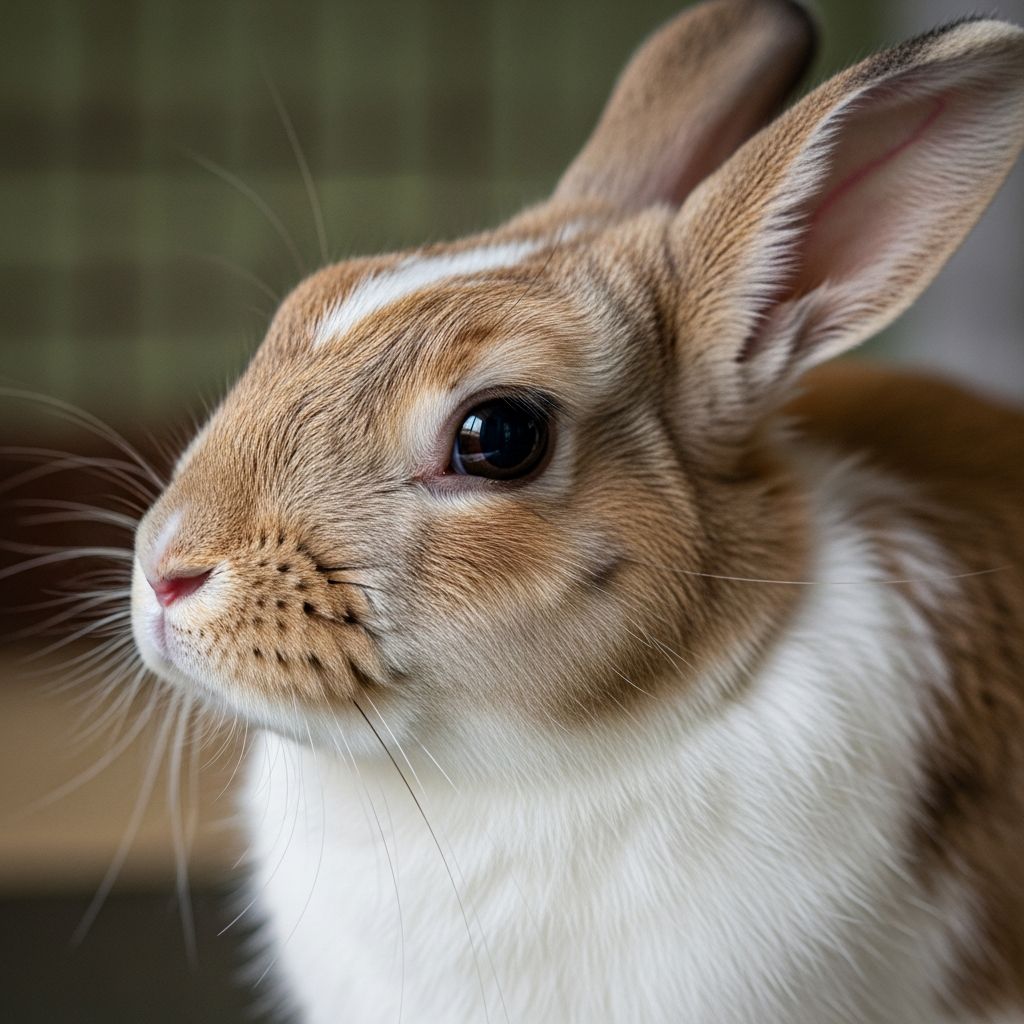
Understanding Encephalitozoonosis in Rabbits
Encephalitozoonosis is a parasitic infection caused by the protozoan parasite Encephalitozoon cuniculi (E. cuniculi), which primarily affects the nervous system and kidneys of rabbits. This intracellular parasite is one of the most common infections affecting domestic rabbits, with studies suggesting that up to 80% of the healthy rabbit population may carry the protozoa without displaying clinical symptoms. While many rabbits remain asymptomatic carriers throughout their lives, some develop serious clinical manifestations that can significantly impact their quality of life. Understanding this disease is essential for rabbit owners who wish to provide appropriate care and early intervention when necessary.
What Causes Encephalitozoonosis?
The Encephalitozoon cuniculi parasite spreads through contact with infected urine, particularly in environments where multiple rabbits coexist. The parasite enters the rabbit’s body through ingestion of contaminated food, water, or fecal material. Once inside the host, the parasite multiplies and spreads throughout the body, primarily targeting the nervous system, brain, kidneys, and eyes. The infection can be transmitted between rabbits through direct contact or environmental contamination, making it particularly concerning in multi-rabbit households or shelter settings.
The parasite’s ability to remain dormant in infected rabbits for extended periods means that seemingly healthy rabbits can still harbor and potentially transmit the infection. This carrier state explains the high prevalence rates observed in rabbit populations, even among animals that never develop clinical disease.
Clinical Signs and Symptoms
The clinical presentation of encephalitozoonosis varies widely depending on which organs are affected and the severity of the infection. The protozoal parasite attacks the nervous system and major organs, causing a diverse range of symptoms.
Neurological Manifestations
The most common and recognizable symptom is head tilt (torticollis or wry neck), which results from inflammation of the vestibular system in the inner ear. Additional neurological signs include circling, rolling, ataxia (loss of coordination), nystagmus (involuntary eye twitching), and general disorientation. Some rabbits experience paresis or paralysis affecting the foreleg, hindleg, or both sides of the body. Seizures may occur in severe cases, and some rabbits display behavioral changes such as excessive lethargy or irritability.
Renal and Hepatic Involvement
The parasite can cause significant kidney and liver damage, leading to organ failure. Affected rabbits may develop calcification within the kidneys, which can be visualized on radiographs. Signs of renal disease include increased thirst and urination, weight loss, and poor coat condition. Liver involvement may result in jaundice and hepatic dysfunction.
Ocular Complications
Eye problems associated with encephalitozoonosis include phacoclastic uveitis (inflammation inside the eye), cataracts, and anterior uveitis. These conditions can lead to significant discomfort and potential vision loss if left untreated.
Other Clinical Signs
Additional symptoms may include incontinence, urinary retention, loss of appetite, and general systemic malaise. The severity and combination of symptoms depend on the stage of infection and individual immune response.
Diagnosis of Encephalitozoonosis
Diagnosing encephalitozoonosis requires a comprehensive approach combining clinical observation, laboratory testing, and imaging studies. A veterinarian experienced with rabbit medicine should perform the diagnostic workup, as proper identification is crucial for determining appropriate treatment protocols.
Serological Testing
Blood tests can detect antibodies against E. cuniculi, indicating either current or past exposure to the parasite. However, antibody presence alone does not confirm active disease, as many healthy carriers will test positive. Paired serum samples taken two weeks apart may demonstrate rising antibody titers, suggesting active infection.
Imaging and Physical Examination
Radiographic and ultrasound imaging can reveal kidney changes, calcification, or other organ involvement. Ophthalmologic examination may identify cataracts or uveitis. Physical examination findings such as head tilt, nystagmus, or ataxia strongly suggest encephalitozoonosis, particularly when combined with positive serological results.
Differential Diagnosis
Other conditions can mimic encephalitozoonosis, including ear infections, stroke, trauma, or toxoplasmosis. Ruling out these alternatives is important before confirming an E. cuniculi diagnosis.
Treatment Options
First-Line Treatment: Fenbendazole
Fenbendazole is the current gold standard for treating encephalitozoonosis and remains the drug of choice for most veterinarians. The standard dosing protocol involves administering 20 mg/kg orally once daily for 28 consecutive days. Fenbendazole works by binding to tubulin in the parasite’s microtubules, disrupting cellular function and preventing reproduction.
Studies have demonstrated that fenbendazole is effective in reducing clinical signs in established infections and can prevent disease in exposed animals when administered prophylactically. Fenbendazole is unique among benzimidazoles in its ability to cross the blood-brain barrier in mammals, allowing it to reach the parasite in neurological tissue. While in rare cases long-term fenbendazole use has been associated with bone marrow failure, digestive problems, or anorexia, these side effects are uncommon when the medication is used at appropriate doses for the standard 28-day treatment period.
Alternative Antiparasitic Agents
Several alternative medications have been explored for rabbits that do not respond to or cannot tolerate fenbendazole. These include albendazole, oxibendazole, ponazuril, and lufenuron, though these are typically reserved for cases that do not respond to standard fenbendazole therapy. Albendazole has shown some efficacy but carries a risk of adverse effects including sudden death and bone marrow failure in some rabbits. Oxibendazole represents another option, though reports increasingly suggest potential parasite resistance may develop with prolonged use.
Anti-Inflammatory Management
Steroids such as dexamethasone or prednisone may be prescribed to reduce central nervous system inflammation during the acute phase of disease, particularly when significant neurological symptoms are present. However, rabbits are extremely sensitive to steroid side effects, and careful risk-benefit analysis must be performed before administration. Non-steroidal anti-inflammatory drugs (NSAIDs) may be used as an alternative to reduce inflammation while minimizing immunosuppression.
Symptomatic Treatment
Beyond antiparasitic therapy, supportive care addresses specific clinical signs. For rabbits experiencing vestibular disease with head tilt or rolling, prochlorperazine or similar medications may help manage vertigo. Benzodiazepines such as midazolam or diazepam can control seizure activity and provide mild sedation for animals with severe vestibular disease. Broad-spectrum antibiotics may be prescribed to prevent secondary bacterial infections.
Supportive Care
Rabbits with severe systemic symptoms require intensive supportive care including fluid therapy to correct dehydration and assisted feeding to ensure adequate nutrition. Syringe feeding high-quality pellets or critical care diet formulas may be necessary for rabbits unable to eat independently due to neurological impairment.
Environmental Management and Prevention
Environmental disinfection is crucial in managing encephalitozoonosis, particularly in multi-rabbit households. The parasite spreads through contact with infected urine, so frequent cage cleaning, disinfection of food and water bowls, and removal of contaminated bedding are essential. Isolating infected rabbits from unexposed animals helps prevent transmission.
For prevention in high-risk situations, prophylactic fenbendazole administration has been shown to be effective in preventing infection in exposed animals. This approach may be recommended in shelter settings or multi-rabbit households when one animal tests positive for E. cuniculi.
Prognosis and Long-Term Outcomes
The prognosis for rabbits with encephalitozoonosis varies considerably depending on disease stage at diagnosis, severity of organ involvement, and individual immune response. Many rabbits live with E. cuniculi their entire lives without displaying any symptoms. With appropriate treatment, rabbits can survive and live normal lives, though some may experience permanent neurological deficits if significant tissue damage has already occurred.
Rabbits diagnosed early in the infection often respond better to treatment than those with chronic disease. However, damage caused by long-standing infection, particularly to the nervous system and kidneys, may not be reversible despite successful antiparasitic therapy. Some rabbits experience complete resolution of clinical signs with treatment, while others may have persistent mild symptoms even after completing the full antiparasitic course.
When to Seek Veterinary Care
Any rabbit displaying sudden onset of head tilt, circling, loss of coordination, or other neurological symptoms should be evaluated by a veterinarian immediately. Similarly, rabbits showing signs of kidney disease, vision loss, or unexplained systemic illness warrant prompt investigation. Early diagnosis and treatment initiation significantly improve outcomes.
Frequently Asked Questions
Q: Can my rabbit transmit E. cuniculi to me or other pets?
A: E. cuniculi is species-specific and cannot be transmitted to humans. It is unlikely to spread to other pet species, though it can spread between rabbits through infected urine and fecal contamination.
Q: Is encephalitozoonosis always fatal?
A: No. Many rabbits carry the parasite without ever developing clinical disease. With appropriate treatment, rabbits can survive and maintain good quality of life. However, some rabbits with severe organ damage may have a poor prognosis despite treatment.
Q: How long does treatment take?
A: Standard fenbendazole treatment lasts 28 days. However, supportive care may be required for weeks or months depending on the severity of clinical signs and response to therapy.
Q: Can my rabbit recover completely?
A: Recovery depends on disease stage and organ involvement. Early-diagnosed cases may resolve completely, while chronic infections may result in permanent neurological or renal changes despite successful antiparasitic treatment.
Q: Should I separate my infected rabbit from other rabbits?
A: Isolation is recommended to prevent transmission to other rabbits. Additionally, strict hygiene protocols including frequent cage cleaning and disinfection are essential to minimize transmission risk.
References
- Encephalitozoon cuniculi – Treatment options for encephalitozoon cuniculi in rabbits — Medirabbit. http://www.medirabbit.com/EN/Neurology/cuniculi/pyrimethamine.htm
- Treatment of Encephalitozoon cuniculi infection in rabbits — Vet Times. 2015-08-10. https://www.vettimes.com/clinical/exotics/treatment-of-encephalitozoon-cuniculi-infection-in-rabbits-cpdrabbits
- Encephalitozoon cuniculi in Rabbits — Bioguardlabs. https://www.bioguardlabs.com/encephalitozoon-cuniculi-in-rabbits/
- A Review of Encephalitozoon cuniculi in Domestic Rabbits — National Center for Biotechnology Information (NCBI). https://pmc.ncbi.nlm.nih.gov/articles/PMC9785705/
- E. cuniculi in Rabbits – Pet Health Information — Mulberry Vets. https://www.mulberryvets.co.uk/pet-advice/e-cuniculi
- E. cuniculi in Rabbits — PetMD. https://www.petmd.com/rabbit/conditions/infectious-parasitic/e-cuniculi-rabbits
Read full bio of medha deb